Article by Ashley Davis, M.S., and Kristine M. Pietsch, M.A.
From the first words we utter, our voice makes us immediately recognizable and identifiable. Our voice is our primary mode of emotional expression — it’s how we connect and communicate with others. Voice is a crucial part of identity.
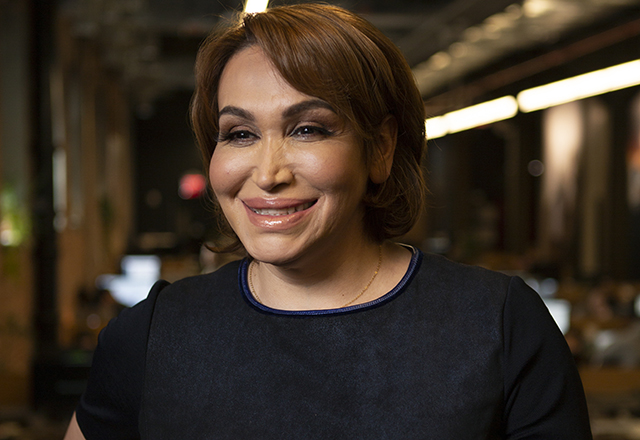
Our Team of Speech-Language Pathologists
We are Ashley Davis (she/her) and Kristine Pietsch (she/her) —speech-language pathologists (SLPs) specializing in voice who work in the Johns Hopkins otolaryngology (ear, nose and throat — ENT) department. We hope to provide insight about the SLP’s role in providing gender affirming voice care, and what clients can expect when working with our team.
As voice therapists, we’re big believers in the power of a team approach to care. We regularly work as part of a multidisciplinary voice team with Johns Hopkins University laryngologists (voice specialist ENTs) to help patients with voice disorders. The Johns Hopkins Center for Transgender Health is made up of surgery, primary care, social work, psychiatry, endocrinology and dermatology providers who are invested in working together to help our clients embody their true selves. At the Johns Hopkins Voice Center, our role is to empower vocal expression in an authentic and effective way.
Voice Therapy for Gender Affirmation — Getting Started
Most clients come to us with the primary goal of modifying the voice to better match their gender identity. When there is a mismatch, it can result in distressing —and sometimes dangerous —mis-gendering and dysphoria. Many have tried some form of voice change before, and we commonly hear complaints of vocal fatigue or discomfort while using a new voice pattern. Vocal strain can easily develop when exploring a different part of the vocal range without guidance.
Voice therapy begins with a conversation to determine what kind of voice the client hopes to target — this target voice may evolve over the course of therapy. Target voices don’t need to emulate what is traditionally masculine or feminine. They can challenge societal concepts of what it means to be feminine, masculine, both, neither or other. Some people aren’t sure what they want at first, and that’s OK. We’re committed to a journey toward discovering what feels right.
Evaluation at our center begins with a review of the client’s medical history, followed by visualization of the vocal folds by the laryngologist and SLP team. As a part of this visit, the client can discuss their vocal identity and expression, and what they hope to gain from voice treatment. Information about vocal fold anatomy, in conjunction with the patient’s goals, helps the team develop a comprehensive treatment plan.
A voice rehabilitation plan sometimes includes voice surgery. When surgery is recommended, voice therapy will continue to play a crucial role in preparing the patient for what to expect, and teaching them to most effectively use their new “instrument” as they heal. In many cases, goals can be achieved with therapy alone.
The first session includes recordings, acoustic and aerodynamic measurements to further define voice characteristics, and a discussion of the personalized training exercises that will help achieve therapy goals. Exercises typically target three primary areas: pitch, intonation and resonance. Pitch and intonation refer to the high and low of the vocal range, and how the client uses their range while speaking. Resonance is a bit more complicated — it involves how a person uses the spaces in their throat, mouth and nose to shape the sound they project, and it is highly influential on the listener’s perception of gender. As needed, we can address intensity, articulation, vocal health and nonverbal communication to further develop the new vocal identity.
Throughout therapy, apps and computer programs are used to track progress, give visual and auditory biofeedback, and provide resources for home practice. For most clients, it takes about three months of regular practice to start to become comfortable with a new vocal range and quality, and up to a year to settle into their new voice and speak without having to think about how they sound. Throughout the process, we troubleshoot challenges and try to address not only how to practice effectively to achieve the desired voice, but also how to “own it.” Session frequency is very client driven — Some people largely practice independently, while others prefer more regular one on one guidance.
What does voice therapy cost?
This is an important question. Voice therapy is less expensive than many transgender health services, but unfortunately that doesn’t mean it’s easily accessible. Under the Affordable Care Act’s antidiscrimination provisions, it’s been illegal since 2010 for federally funded clinics or programs to deny patients service based on their gender identity. Despite this, many of our clients struggle to get their treatment covered by insurance because insurance companies sometimes try to classify speech therapy as cosmetic.
The laryngologist will enter the recommendation (otherwise known as an “order”) for voice therapy into the patient’s chart during the initial evaluation, but this doesn’t mean the service will be fully covered. We provide procedure and diagnosis codes for the client to call the insurance company and inquire about coverage. As a future goal, our team hopes to be able to offer a hybrid group/individual therapy model that would be affordable/sliding scale fee based and provide greater accessibility to care and treatment.
We are always happy to answer any questions about voice therapy and treatment. We’re passionate about supporting people who are transgender as they place their trust in us and develop their voices during their gender affirmation journey.